
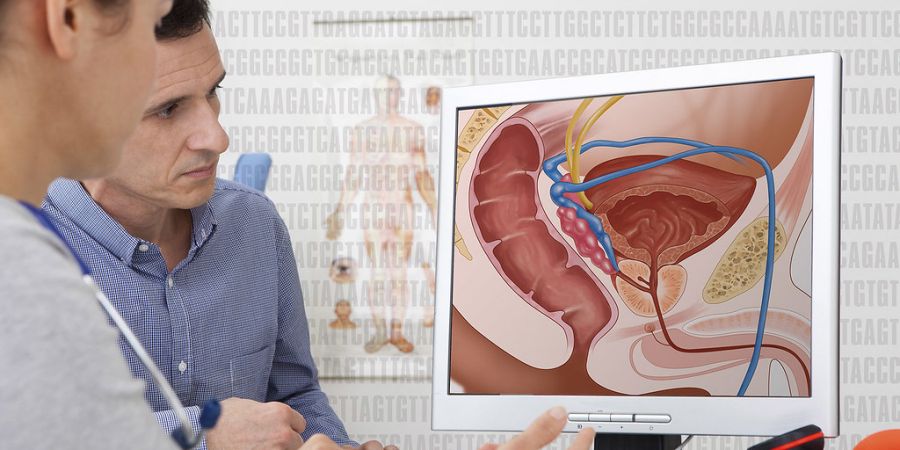

Prostate cancer originates from cells present within a gland, the prostate, which begin to grow uncontrollably. The prostate is present only in men, is positioned in front of the rectum and produces a portion of seminal fluid (sperm), which mixes with the spermatozoa and is expelled during ejaculation.
Under normal conditions, the prostate is the size of a walnut, but over the years, or due to some pathologies, it can enlarge, grow, giving mainly urinary disorders.
This gland is very sensitive to the action of hormones, especially male ones, such as testosterone, which affect its growth.
It is one of the most common cancers in men and accounts for about 20 percent of all cancers diagnosed in humans.
This is also evidenced by data on the number of people still alive five years after diagnosis - an average of 91 percent - one of the highest percentages in the case of cancer, especially if we consider the average age of patients and other causes of cancer—possible death.
According to the latest data, about one in 8 men in our country are likely to have prostate cancer in their lifetime.
Who is at risk for prostate cancer?
One of the main risk factors for prostate cancer is age: the chances of getting sick are very low before the age of 40 but increase significantly after the age of 50, and about two out of three cancers are diagnosed in people over the age of 65.
Researchers have shown that about 70 percent of men over the age of 80 have prostate cancer, although in most cases, the disease shows no signs of itself and is only found at an autopsy after death.
When it comes to prostate cancer, another negligible factor is undoubtedly familiarity: the risk of getting sick is twice as high for those who have a sick blood relative (father, brother, etc.), in comparison to those who have no case in the family.
The presence of mutations in some genes, such as BRCA1 and BRCA2, already involved in the development of breast and ovarian cancer, or the HPC1 gene, may also increase the risk of prostate cancer.
The chance of getting sick can also be linked to high levels of hormones such as testosterone, which stimulates prostate cell growth, and insulin-like hormone IGF1, which works for cell growth rather than sugar metabolism.
No less important are the risk factors related to lifestyle: a diet rich in saturated fats, obesity, lack of physical exercise are just some of the unhealthy characteristics and habits increasingly prevalent in the western world, which may favor the development and growth of prostate cancer.
Prostate cancer and its types
There are several types of cells in the prostate, each of which can transform and become cancerous; almost all diagnosed prostate cancers originate from epithelial cells and are consequently called adenocarcinomas (like all cancers that originate from single epithelial cells).
In addition to adenocarcinoma, sarcomas, small cell carcinomas, and transient cell carcinomas can also be found in rare cases in the prostate.
Much more common than carcinomas are benign pathologies that affect the prostate, especially after the age of 50, and that sometimes cause symptoms that can be confused with those of the tumor. In benign prostatic hyperplasia, the central part of the prostate enlarges, and the overgrowth compresses the urethra.
This channel carries urine from the bladder to the external environment through the prostate. This compression of the urethra, on the part of the enlarged prostate, creates problems during the passage of urine through the ureters, such as waiting to urinate (hesitation), pain (dizziness), cessation of urination, etc.
Prostate Cancer: Signs and Symptoms
In the early stages, prostate cancer is asymptomatic. It is diagnosed after a urological examination, which includes digital-rectal examination or PSA control, using a blood sample.
When the tumor mass increases, it causes urinary symptoms:
Urinary symptoms can often be related to benign prostate problems, such as hypertrophy. In any case, it is helpful to contact your doctor or urologist, who will decide if further examinations are needed.
Prostate Cancer and its Prevention
There is no specific primary prevention for prostate cancer. Still, there are some helpful rules of conduct that can be easily followed in daily life: increase consumption of fruits, vegetables, whole grains and reduce the use of red meat, especially if patients are very naturally obese, avoid foods high in saturated fat.
Secondary prevention involves contacting the doctor and preferably performing a urological examination every year if the patient is already familiar with the disease or if he has urinary disorders.
Prostate cancer and its diagnosis
The number of prostate cancer diagnoses has increased steadily since the PSA test was approved by the US Food and Drug Administration (FDA) in the 1990s. At its real value to diagnose a tumor, however, the debate is open as values often change due to the presence of benign hyperplasia or an infection.
For this reason, in recent years, a decrease in the use of this test has been observed. In particular, serum PSA measurement should be carefully evaluated based on the patient's age, familiarity, exposure to any risk factors, and clinical history.
Urinary symptoms of prostate cancer appear only in the later stages of the disease and, in any case, may also indicate the presence of various tumor diseases. Therefore, the diagnosis must be made by a specialist doctor who considers several factors before deciding how to act.
How to treat prostate cancer?
There are many types of prostate cancer treatment available today, each with specific benefits and side effects. Only a careful analysis of the patient's characteristics (age, longevity, etc.) and disease (low, medium or high risk) will allow the urologist to recommend the most appropriate and personalized strategy by also agreed on preferential therapy, who should undergo treatment.
Prostate cancer therapy may include: observation, untreated surgery, radiation therapy, high-intensity focused ultrasound (HIFU), chemotherapy, cryosurgery, hormone therapy, or a combination of these. Choosing the best option depends on the stage of the disease, Gleason score, and PSA levels. Other important factors are the age of the patient, his general condition and his opinion about the proposed therapy and possible side effects. Since all therapies can cause significant side effects, such as erectile dysfunction and urinary incontinence, discussing possible therapy with the patient often helps therapeutic balance goals with the risks of lifestyle change.
When it comes to active therapy, the choice often falls on radical surgery. Radical prostatectomy - removing the entire prostate gland and lymph nodes in the region near the tumor - is considered a curative procedure if the disease is confined to the prostate.
In many western countries, robots suitable for practicing intervention are becoming more widespread. However, recent studies have shown that the results of the robotic and classical intervention are equivalent over time: therefore, there is no real indication to perform interference using a robot.
For advanced cancers, the scalp (scalp) often fails to cure the disease and therefore needs a combination of treatments such as radiotherapy or hormone therapy.
For the treatment of prostate cancer, in the treatments considered standard, it has also been shown that external beam radiotherapy is quite effective, in low-risk tumors, with results similar to those of radical prostatectomy.
Another radiotherapy technique that seems to offer similar results to previous low-risk diseases is brachytherapy, which inserts small "seeds" that emit radiation into the prostate. When prostate cancer is metastatic, unlike what happens in other cancers, chemotherapy is not the treatment of the first choice, and hormone therapy is preferred.
This aims to reduce the level of testosterone - the male hormone that stimulates the growth of prostate cancer cells - but brings with it side effects such as decreased or extinguished sexual desire, impotence, hot flashes, weight gain, osteoporosis, weight loss: muscle mass and fatigue.
If cancer has spread beyond the prostate, treatment options vary. Hormone therapy and chemotherapy are often reserved for cases where the disease has spread beyond the prostate; however, there are exceptions: radiotherapy can be used for some advanced cancers and hormone therapy for some at an early stage.












